What is Healthcare Revenue Cycle Management?
Inefficient billing processes, unclear statements, and poor communication regarding financial responsibilities can lead to patient dissatisfaction. Without adopting patient-centric healthcare revenue cycle management healthcare processes, including revenue cycle management training and courses, healthcare organizations may struggle to provide transparent and convenient billing experiences, potentially harming their reputation and patient relationships. Enhancing patient satisfaction through streamlined financial operations is crucial for improving the patient satisfaction score.
so here is the solutions:
what is rcm in healthcare?
Revenue cycle management (RCM), also known as RCM, is the comprehensive process of managing the administrative and clinical functions associated with capturing, managing, and collecting patient service revenue in the healthcare industry. It encompasses the entire life cycle of a patient account, from initial registration and appointment scheduling to final payment collection and revenue realization. This makes it a cornerstone of healthcare RCM, including what is revenue cycle management, what is revenue cycle in healthcare, and the RCM in medical billing
revenue cycle managment is a complex and multifaceted process that involves several interconnected steps, each playing a crucial role in ensuring accurate billing, maximizing reimbursements, and maintaining financial viability for healthcare providers. Understanding the revenue cycle processes in healthcare is essential for effective revenue cycle management.
revenue cycle management steps:
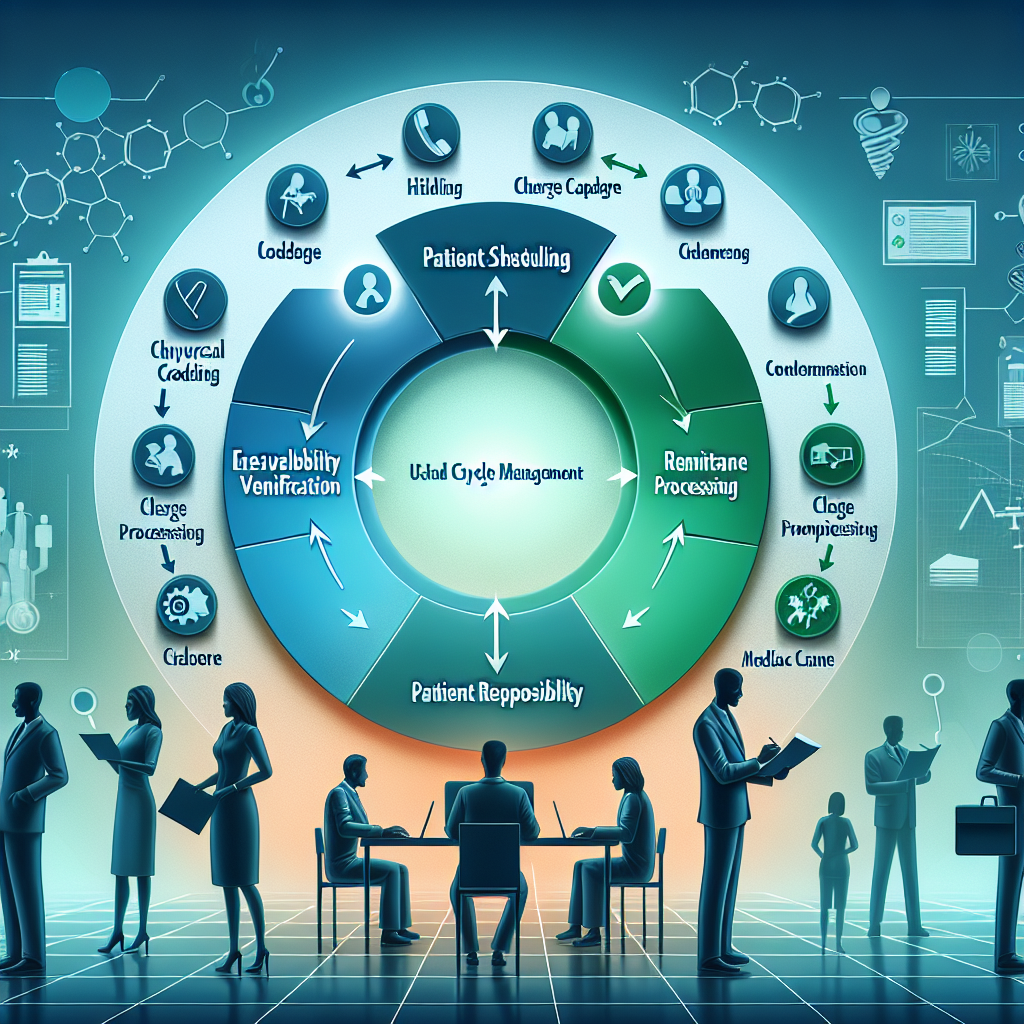
⦁ Patient Registration and Eligibility Verification
⦁ Medical Coding and Charge Capture
⦁ Claim Submission and Tracking
⦁ Payment Posting and Remittance Processing
⦁ Denial Management and Appeals
⦁ Patient Billing and Collections
⦁ Reporting and Analytics
Effective revenue cycle management services are critical for healthcare organizations as they directly impact their financial performance, operational efficiency, and compliance with regulatory requirements. A well-managed revenue cycle can lead to improved cash flow, reduced administrative costs, minimized denials and underpayments, and enhanced patient satisfaction. Achieving these goals often requires revenue cycle management certification, training, and courses to set performance benchmarks in hospital revenue cycle management.
However, the complexity of the healthcare system, coupled with stringent regulations, evolving payer rules, and increasing patient financial responsibility, makes medical revenue cycle management a challenging endeavor. Healthcare providers often leverage technology solutions, such as medical billing software, electronic health records (EHRs), and healthcare data analytics tools, to streamline processes, improve accuracy, and ensure healthcare compliance.
what is rcm in medical billing?
Effective RCM cycle in medical billing is crucial for healthcare providers to maintain financial health, ensure regulatory compliance, and deliver a positive patient experience. By implementing best practices, leveraging technology solutions, and fostering a culture of continuous improvement, healthcare organizations can optimize their medical billing revenue cycle, maximize reimbursements, and achieve long-term financial sustainability.
Key Components of Revenue Cycle Management
Patient Access and Registration: This involves collecting accurate patient demographic and insurance information during the initial registration process, as well as verifying insurance eligibility and benefits, ensuring a smooth start to the patient eligibility verification process. Proper identification during preregistration is key to this phase, highlighting the importance of efficient registration processes.
1. Medical Coding and DocumentationSkilled medical coders translate clinical documentation into standardized codes that facilitate accurate billing and reimbursement, a critical step in medical billing and coding. This expertise ensures that healthcare services are coded correctly, streamlining the billing process and emphasizing the vital role of coding.
2. Charge Capture:Ensuring all services, procedures, and supplies provided to the patient are accurately recorded and billed is fundamental to managing billable charges and charge entry efficiently. This requires a solid foundation in medical billing knowledge and an understanding of medical records documentation to ensure accuracy and compliance.
3. Claim Submission and Follow-up:Submitting claims to health insurance companies or government programs and tracking outstanding claims, denials, or delays is a crucial part of the billing process, ensuring that healthcare providers are reimbursed for their services. Maintaining a high clean claim rate is essential for financial health, underscoring the importance of coding and compliance practices.
4. Payment Posting and Remittance: Accurately posting payments from payers to patient accounts and reconciling remittance advice (explanations of payment) are key steps in the billing process, ensuring that patient payments are correctly applied. This careful collection and reconciliation support the overall patient revenue cycle, emphasizing the need for balance in financial dealings.
5. Denial Management: Analyzing denied claims, identifying root causes, and managing the appeals process with a meticulous focus on coding ensures that every aspect of coding is scrutinized to secure the rightful reimbursement for healthcare services. This approach guarantees that healthcare providers receive appropriate compensation for their services.
6. Patient Billing and Collections: Generating accurate patient statements, providing clear explanations of financial responsibility, and managing payment collections.
7. Analytics and Reporting:Collecting and analyzing healthcare data to monitor key performance indicators, identify opportunities for optimizing the revenue cycle for better profitability, and support strategic decision-making is crucial. This process helps in pinpointing areas prone to revenue leakage and devising strategies to mitigate these losses, ensuring a more profitable operation.
Successful Revenue Cycle Management (RCM) requires collaboration among various stakeholders, including front-end staff, medical coders, billers, financial counselors, and revenue cycle managers. It also necessitates continuous process improvement, staff training, and a commitment to adopting best practices and industry standards in healthcare compliance and management, with a particular emphasis on coding.
As the healthcare landscape continues to evolve, understanding revenue cycle management and its effective implementation remains a critical component of operational success for healthcare providers, ensuring financial sustainability and enabling the delivery of high-quality patient care.
Advantages of Revenue Cycle Management

Revenue cycle management (RCM) offers numerous advantages for healthcare providers, contributing to their financial well-being, operational efficiency, and overall success. These advantages underscore the importance of optimizing revenues to sustain healthcare practices.
Maximized Revenue Capture:
One of the primary advantages of effective RCM is maximized revenue capture. By optimizing processes such as medical coding, charge capture, claim submission, and denial management, healthcare organizations can ensure they receive appropriate reimbursement for all services rendered. This strategic approach leads to increased revenue collection and improved cash flow.
Reduced Administrative Costs:
RCM streamlines and automates many administrative functions, minimizing manual efforts, reducing errors, and enhancing productivity. This includes processes like eligibility verification, claim scrubbing, payment posting, and reporting, thereby reducing administrative overhead and realizing significant cost savings through efficient management of both back-end processes and front-end operations.
Improved Regulatory Compliance:
The healthcare industry is subject to a complex web of regulations and guidelines, including those related to medical coding, billing practices, patient privacy (HIPAA), and payer requirements. Robust RCM processes and systems help healthcare organizations maintain compliance practices, mitigating the risk of costly penalties and legal consequences.
Enhanced patient Satisfaction:
RCM focuses on delivering transparent and convenient billing experiences for patients. Clear statements, accessible payment options, and effective communication regarding financial responsibilities contribute to improved patient satisfaction scores and stronger provider-patient relationships.
Data-Driven Decision Making:
RCM processes generate a wealth of data and insights related to key performance indicators, such as claim denials, payment delays, underpayments, and revenue cycle leakage. Advanced analytics and reporting capabilities within RCM systems enable data-driven decision-making, allowing healthcare organizations to identify areas for improvement, forecast financial performance, and make informed strategic decisions through effective management.
Scalability and Growth Support:
As healthcare organizations expand their operations, patient volumes, and service offerings, robust and scalable healthcare RCM processes become essential to handle this growth efficiently. Effective RCM ensures financial control, operational efficiency, and regulatory compliance are maintained during periods of expansion, safeguarding the financial operations of these institutions.
Competitive Advantage:
By optimizing their revenue cycle management, healthcare providers can gain a competitive advantage over those with inefficient processes. Improved financial performance, operational efficiency, and patient satisfaction can differentiate providers in the healthcare RCM landscape, attracting more patients and payers and boosting revenue generation.
Focus on Core Competencies:
Effective RCM frees up healthcare organizations to focus on their core competencies - delivering high-quality patient care and medical services. By outsourcing or streamlining administrative and financial functions, providers can allocate more resources to their primary mission, enhancing patient services and reinforcing their role as a healthcare provider, especially in ambulatory care and other healthcare facilities.
In short, understanding what is revenue cycle management reveals numerous advantages that contribute to the financial sustainability, operational efficiency, and overall success of healthcare providers. By leveraging best practices, technology solutions, and specialized expertise in healthcare RCM, organizations can optimize their financial performance and enhance their ability to deliver exceptional patient care.
The Crucial Role of Revenue Cycle Management in Healthcare Amidst the COVID-19 Pandemic:
Revenue cycle management in healthcare has emerged as a critical component, particularly during the COVID-19 pandemic year of 2020, offering indispensable solutions to address the financial uncertainties faced by healthcare providers. RCM systems, including RCM medical billing, play a pivotal role in maintaining financial stability by optimizing revenue streams and streamlining RCM billing processes despite challenges such as reduced patient volumes and escalating costs of supplies. These systems expedite billing and claims processing, ensuring accuracy in submissions and facilitating swift patient payments. Moreover, RCM platforms enhance patient engagement through user-friendly interfaces, enabling seamless communication and remote access to services. Additionally, they aid healthcare organizations in staying compliant with evolving regulations and leveraging data analytics for informed decision-making, thereby fortifying their resilience in navigating unprecedented challenges.
Without RCM OR With RCM differnce in Healthcare Industry As per global rcm average analysis:
Details:
Total Revenue Generated: The hospital's revenue increased from $5,000,000 without RCM to $6,500,000 with RCM, resulting in a difference of $1,500,000, showcasing the impact of effective revenue generation strategies.
Cash Flow: Cash flow improved from $800,000 without RCM to $1,200,000 with RCM, reflecting a difference of $400,000.
Accounts Receivable Days: With RCM, the accounts receivable days decreased from 60 days to 45 days, indicating a more efficient billing and payment collection process.
Denial Rate: The denial rate decreased from 12% without RCM to 8% with RCM, representing a reduction of 4% in denied claims, thanks to improved coding practices.
Patient Satisfaction Score: Patient satisfaction scores increased from 7.5 without RCM to 8.7 with RCM, showcasing a notable improvement of 1.2 points in patient experience and underscoring the importance of patient satisfaction in healthcare.

.png)

.png)

This comment has been removed by the author.
ReplyDelete